Science of Using CGMs for Weight Loss

Learn how the food you eat, the way you exercise, your sleep quality, and your stress patterns affect your blood sugar (glucose). Incorporate changes to your nutrition and lifestyle to keep your glucose stable. Practice these new habits every day and achieve better health, weight loss, and more.
This is the Signos approach to healthy weight loss.
Our unique-to-you program for weight loss is backed by a growing field of scientific research—and more studies are coming out all the time.
Read the latest scientific evidence for using CGMs for weight loss.
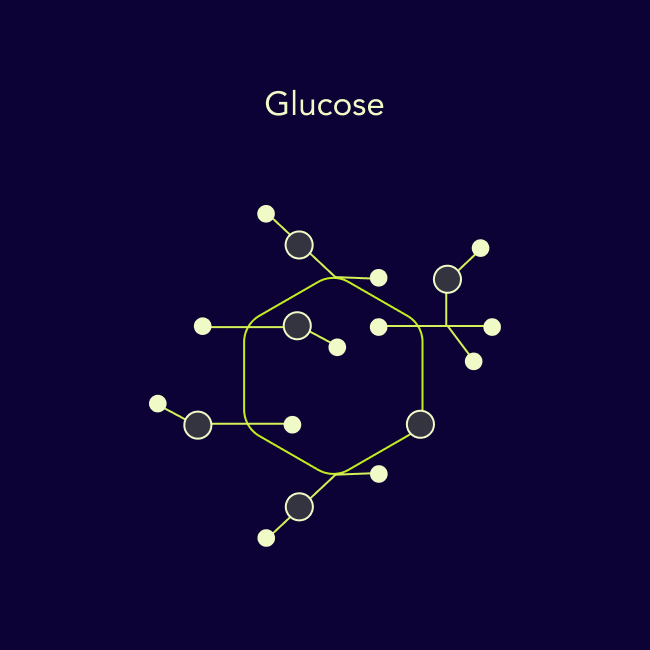
What is glucose?
Glucose is carried to the cells through the bloodstream. Several hormones, including insulin, control glucose levels in the blood.
Read more (0 articles)
Roles of the Gut in Glucose Homeostasis
Many foods that you eat can increase your glucose. Your body has a complex hormonal response to keep glucose relatively in a “normal” range. However, excess fat, insulin resistance, pre-diabetes, and other factors are associated with higher, longer glucose spikes.
Personalized Nutrition by Prediction of Glycemic Responses
People have unique glucose responses to food; scientists noted a “high variability in response to identical meals, suggesting that universal dietary recommendations may have limited utility.” This research supports the idea that each person can respond differently to food, food combinations, and the context in which the food was consumed.
Does Hunger and Satiety Drive Eating Anymore? Increasing Eating Occasions and Decreasing Time Between Eating Occasions in the United States
Americans eat and drink more frequently than they did 30 years ago; this increases the number of times a day that blood glucose will rise and may indicate an overall increase in energy intake.


How glucose can impact health
Glucose spikes—or a rapid rise in the amount of glucose in the body—cause proportional insulin release. Glucose that isn’t used by activity gets stored for later use, sometimes as fat.
Read more (0 articles)
Real-Life Glycaemic Profiles in Non-Diabetic Individuals with Low Fasting Glucose and Normal HbA1c: The A1C-Derived Average
Even healthy people can have high and unpredictable glucose spikes, which get larger and more unpredictable if you develop impaired glucose tolerance (often due to excess fat and insulin resistance).
Insulin Translates Unfavorable Lifestyle into Obesity
When glucose is elevated, insulin gets released by the pancreas to move the glucose into cells for immediate energy. Glucose that isn’t used gets stored for later, often as fat in our tissues. Sugar and fat eaten together also accelerates fat storage. Results of several studies indicate that insulin levels may predict obesity in children and adolescents.
Glucose Characteristics in Normal Glucose Tolerance Subjects with Metabolic Syndrome
Inability to regulate glucose is associated with metabolic syndrome and elevated glucose levels, which raises the risk for heart disease, type 2 diabetes, obesity, and more.
Effects of Dietary Glycemic Index on Brain Regions Related to Reward and Craving in Men
Post-meal high glucose responses can lead to the “crash” effect, where your glucose spikes then drops quickly. This also stimulates reward behavior in your brain, which increases the chance that you’ll want to eat more high-glycemic foods
Acute Effect of Meal Glycemic Index and Glycemic Load on Blood Glucose and Insulin Responses in Humans
High glycemic load meals cause high glucose and high insulin levels: “virtually a straight-line relationship between the meal [glucose load] and serum glucose and insulin responses was found.”

weight gain since March 2020
"Glucose stabilization is the key for successful and sustainable weight loss."

"People need a personalized solution for weight management. The Signos platform can help people short-circuit the cycle of excess weight, glucose intolerance, insulin resistance, and the storage of excess dietary glucose and triglycerides as fat.
The best 'diets' are the ones that make you lose weight and that you can sustain. The most effective weight loss apps are the ones that hold you accountable and encourage behavior change.
Glucose is the key link for successful weight loss and mobile engagement—it provides real-time feedback while the app experience builds accountability and instigates sustainable lifestyle change that can result in weight loss."

Sustainable weight loss
The cells in your brain sense changes in your blood glucose and alter your appetite accordingly. Swings in your blood sugar can make you hungry and more likely to overeat. When your glucose stays stable, your brain sends satiety signals and reduces hunger levels.
Read more (0 articles)
Effect of the glycemic index of the diet on weight loss, modulation of satiety, inflammation, and other metabolic risk factors: a randomized controlled trial
A low-GI and energy-restricted diet containing moderate amounts of carbohydrates may be more effective than a high-GI and low-fat diet at reducing body weight and controlling glucose and insulin metabolism.
Return of Hunger Following a Relatively High-Carbohydrate Breakfast Is Associated with Earlier Recorded Glucose Peak and Nadir
When a group of overweight, healthy adults consumed a low-fat, high-carb breakfast, they experienced higher post-meal insulin, a more rapid rise and fall in peak glucose, and more hunger at 3-4 hours after the meal compared to a group that ate a high-fat, low-carb breakfast. The rise and fall in glucose (versus the total concentration of glucose) likely explained the earlier return of hunger in the low-fat, high-carb group.
Postprandial Glycaemic Dips Predict Appetite and Energy Intake in Healthy Individuals
Fluctuations of glucose throughout the day are normal to a certain degree, but small spikes and dips may influence behavior. A 2021 study of people under real-world conditions, wearing continuous glucose monitors, showed that lower glucose dips following a meal were predictive of eating sooner and eating more calories at that subsequent meal.
Low glycemic load experimental diet more satiating than high glycemic load diet
We investigated the effect of low and high glycemic load (GL) diets on satiety and whether satiety varied by body mass index (BMI), gender, and serum leptin. In summary, reducing GL, and/or increasing fiber, may be an effective way to lower calories consumed, improve energy balance, and ultimately reduce cancer risk.
Insulin Resistance and Inflammation Predict Kinetic Body Weight Changes in Response to Dietary Weight Loss and Maintenance in Overweight and Obese Subjects by Using a Bayesian Network Approach
Study participants with higher baseline insulin levels and inflammation showed decreased weight loss during a calorie-restricted diet—and were more prone to regaining weight lost after the diet.
Glycemic Load, Exercise, and Monitoring Blood Glucose (GEM): A Paradigm Shift in the Treatment of Type 2 Diabetes Mellitus
Newly diagnosed patients with type 2 diabetes reported a 4% body weight loss over 6 months from avoiding high-glycemic foods, eating foods that don’t cause large glucose spikes, including physical activity, and monitoring glucose levels via fingerstick. Weight loss was not a focus in this study, but patients who followed the GEM paradigm (glycemic load, exercise, monitor glucose) showed that addressing high sugar intake led to weight loss.
Effects of dietary glycemic index on brain regions related to reward and craving in men
Compared with an isocaloric low-GI meal, a high-GI meal decreased plasma glucose, increased hunger, and selectively stimulated brain regions associated with reward and craving in the late postprandial period, which is a time with special significance to eating behavior at the next meal.
Genetic Evidence That Carbohydrate-Stimulated Insulin Secretion Leads to Obesity
This research supports a causal relationship between genetically determined glucose-stimulated insulin secretion and obesity. A lifetime of consumption of foods with a high-glycemic load promotes weight gain through the anabolic effects of increased insulin secretion.
Continuous Glucose Monitoring in the Self-Management of Type 2 Diabetes: A Paradigm Shift
Study participants followed the GEM paradigm using continuous glucose monitors instead of self-monitored glucose checks. Participants had an average 17-pound (7%) weight loss over 3 months, with significant reductions in BMI, blood pressure, and other health markers.
A High Glycemic Meal Suppresses the Postprandial Leptin Response in Normal Healthy Adults
High-glycemic foods suppress leptin, a hormone that helps regulate energy balance by inhibiting hunger. Lower post-meal insulin and higher leptin levels suggest that low-glycemic meals instigate a metabolic response that encourages people to eat less.
A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial
Compared with a low-fat diet, a low-carbohydrate diet program had better participant retention and greater weight loss. During active weight loss, serum triglyceride levels decreased more and high-density lipoprotein cholesterol level increased more with the low-carbohydrate diet than with the low-fat diet.



Consistent energy and improve mood
When you eat high-glycemic foods, your glucose spikes and then dips. Do this several times a day and your energy will bob up and down too. Stable glucose enables you to have consistent energy levels throughout the day.
Read more (0 articles)
Subjective Mood and Energy Levels of Healthy Weight and Overweight/Obese Healthy Adults on High- and Low-Glycemic Load Experimental Diets
In healthy adults—but especially overweight and obese people—a high-glycemic diet was associated with higher depression symptoms, mood disturbance, and fatigue compared to a low glycemic-load diet.
Does Glycemic Variability Impact Mood and Quality of Life?
Greater glycemic variability may be associated with lower quality of life and negative moods, scientists reported when they monitored 23 women with type 2 diabetes who wore continuous glucose monitors.

How CGM use can improve health outcomes
Continuous Glucose Monitor (CGM) benefits extend beyond revealing glucose numbers. Studies show that CGM use can encourage behavior changes that lead to weight loss, adherence to an exercise regimen, and improved nutrition.
Read more (0 articles)
Use of a Real Time Continuous Glucose Monitoring System as a Motivational Device for Poorly Controlled Type 2 Diabetes
A study of patients with poorly controlled type 2 diabetes showed that participants who used continuous glucose monitors (vs. finger sticks) for just nine days over the course of three months lost about 5 pounds, decreased calorie intake, and increased weekly exercise time. Even intermittent use of a CGM showed potential to incorporate lifestyle changes that lead to weight loss.
Self-Monitoring Using Continuous Glucose Monitors with Real-time Feedback Improves Exercise Adherence in Individuals with Impaired Blood Glucose: A Pilot Study
Individuals with prediabetes or type 2 diabetes were separated into two 8-week study groups: one in a standard care exercise program and the other in a program where participants were taught how to use a continuous glucose monitor to observe how exercise affects blood glucose. The CGM group showed greater increases in self-efficacy, goal setting, and time interactions for self-monitoring. Both groups experienced improved waist circumference, fitness, and health-related quality of life.
Glucotypes Reveal New Patterns of Glucose Dysregulation
A study showed that of 57 people wearing CGMs, and who were considered to have a normal glucose tolerance by normal standards, subjects were found to have elevated blood glucose in the prediabetic range 15% of the time and in the diabetic range 2% of the time.
Continuous Glucose Monitoring With Low-Carbohydrate Diet Coaching in Adults With Prediabetes: Mixed Methods Pilot Study
This study examines the use of CGMs in coordination with low-carb diet coaching to drive dietary behavior change. Those who found it easier to use the CGM and follow the low-carb diet lost more weight than those who did not.
Behavior Modification in Prediabetes and Diabetes: Potential Use of Real-Time Continuous Glucose Monitoring
This review emphasizes the role continuous glucose monitors can play in lifestyle changes, weight reduction, and the potential to decrease the use of insulin and other medications in patients with types 1 and 2 diabetes and prediabetes.
Continuous Glucose Monitoring Counseling Improves Physical Activity Behaviors of Individuals with Type 2 Diabetes: A Randomized Clinical Trial
Diabetic study participants who were given continuous glucose monitors to wear for 8 weeks showed higher self-efficacy for sticking to regular physical activity without relapse than a control group.





